The Lancet recently published an article series “A call for action” on chronic back pain questioning widely used ineffective and even dangerous treatments. One of the articles outlines the latest guidelines adopted in many countries. At the top of the list are cognitive support, advice to stay active and exercise: “Recommendations include use of a bio-psychosocial framework to guide management with initial non-pharmacological treatment, including education that supports self-management and resumption of normal activities and exercise. Guidelines recommend prudent use of medication, imaging, and surgery.”
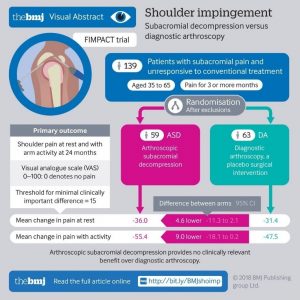
A number of recent studies have shown that many surgeries used routinely for shoulder impingement, meniscal tears and others have no scientific justification. Active physical therapy and even sham surgery produced the same outcomes in long term follow-ups.
With this surge of new guidelines and evidence supporting exercise as therapy you would think that concepts like Active Physiotherapy, Exercise Therapy or Medical Exercise are already well defined. But the truth is that there are no real definitions that would allow systematic adoption of the best practices and tools. Methods and tools vary from country to country and therapist to therapist.
David Health Solutions Ltd. has for years developed systematically tools, data collection and methodology for various musculoskeletal problems. One could argue that it is perhaps the only global exercise method (especially for the spine) that has been systematically adopted with similar protocols all over the world. Nobody knows exact numbers (intelligent devices were introduced in 2013) but it is safe to say that several million patients have been successfully treated using our technology and protocols.
Several million patients have been treated using our technology and protocols.
With the abundance of experience and a number of third-party studies we can claim with confidence that data-driven, device-based exercise therapy will fundamentally change the way most of spine and orthopedic problems are going to be treated in the future. I will support my claim with 7 facts that anybody can easily verify.
1. Device-based exercise therapy can be quantified
What I mean by quantification is that all parameters of the exercises are controlled numerically so that program creation, patient guidance as well as data collection can be digitally managed. This is the only way we can develop structured programs based on the individual’s baseline tests, background data and severity level of the problem and all this in mass scale.
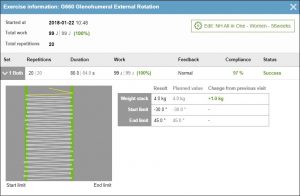
As an example we are not interested in exercising external rotation of the shoulder as a qualitative description. We want to exercise the shoulder rotation e.g. from -30 degrees to 45 degrees at a speed of 37,5 degrees per second with a load of 15% from the 1RM for 84 seconds while the shoulder is in 60-degree abduction. Above you can see an example of a near perfect result from an 86-year-old woman.
It is easy to understand the benefits of quantification. First, it is possible to save an incredible amount of time when a complete program can be populated in seconds based on the client’s strength and mobility tests, which are performed with the same devices. Once the program is generated, it is easy to verify its suitability during the first introductory session and make necessary fine tuning directly from the device terminals.
Second, we can learn. Think about it: 1) we know the patient’s demographics, baseline questionnaires, pain values and physical test values; 2) we know the intervention exactly down to a single repetition including any additional free exercising or relaxation which are documented as well; and 3) we know the outcome. This gives us unprecedented possibility to understand what works and what does not work. With hundreds of thousands of patient cases already in the database with quality data, we are now moving to the next phase using AI to learn the best treatment pathways for each individual. Our dream has always been to provide the exact right treatment for each patient. Now this is truly becoming a reality.
2. Optimal neuromuscular innervation can be produced with joint-specific resistance control
This would seem like a self-evident fact, but the reality is far from it. Most exercises are in fact very poor in terms of resistance control regardless if we talk about functional movements or devices. Every joint moves around its axis using muscles with a particular biomechanical model and each muscle has its own strength-length relationship. These two form the “strength curve” of that joint meaning that a certain amount of force can be produced at each degree of angle of the movement. The strength curve varies depending if the force is measured isometrically or during the concentric or eccentric phases of the movement. Even the level of fatigue has an effect on what this strength curve looks like.
Let’s take a practical example: a typical exercise is the external rotation of the shoulder using a rubber band. As we all know the resistance of a rubber band increases as it is stretched. But the strength in this movement is in fact rapidly decreasing towards the end of the movement. And what is the effect of having the highest resistance at the weakest point of the movement? Either the resistance in the strongest area of the movement is hopelessly insufficient or the resistance at the weakest area is so high that the patient has to cheat. And this is what often happens especially when pain is involved.
We have validated our “variable resistance” principle already in the 80’s. This method means that the loading optimally corresponds the strength at each point of the movement with a joint specific cam that regulates the resistance. Correctly designed variable resistance has an incredible ability to innervate muscle activity and produce fatigue. This is a direct quotation from one of the validation studies: “The present findings suggest that repeated concentric contractions of the knee extensors against a variable resistance may create optimal conditions which may result in great fatigue effects on the neuromuscular system” (Electromyogr. Clin. Neurophysiol. 28(2-3):79-87 · March 1988)
Let’s take a practical example: a typical exercise is the external rotation of the shoulder using a rubber band. As we all know the resistance of a rubber band increases as it is stretched. But the strength in this movement is in fact rapidly decreasing towards the end of the movement. And what is the effect of having the highest resistance at the weakest point of the movement? Either the resistance in the strongest area of the movement is hopelessly insufficient or the resistance at the weakest area is so high that the patient has to cheat. And this is what often happens especially when pain is involved.
We have validated our “variable resistance” principle already in the 80’s. This method means that the loading optimally corresponds the strength at each point of the movement with a joint specific cam that regulates the resistance. Correctly designed variable resistance has an incredible ability to innervate muscle activity and produce fatigue. This is a direct quotation from one of the validation studies: “The present findings suggest that repeated concentric contractions of the knee extensors against a variable resistance may create optimal conditions which may result in great fatigue effects on the neuromuscular system” (Electromyogr. Clin. Neurophysiol. 28(2-3):79-87 · March 1988)
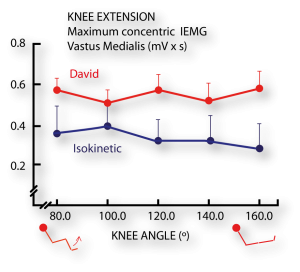
Another study demonstrated that variable resistance generated high EMG activity distributed evenly over the whole range of motion. An interesting observation was that with the same maximal effort by the test persons, isokinetic device produced as much as 40% lower EMG levels. This shows that artificial resistance (not gravity-based loading) is unable to innervate muscles properly.
So what are the practical benefits of having precise resistance control? First, patients feel that the movement is very gentle and smooth, no jerks or peaks. Second, regardless of the loading level muscles are always doing the most amount of work possible on that level. Third, even when the fatiguing effect is very high, exercise is safe. Fourth, when the joint is supported and the load is smooth, exercising is practically always pain free.
3. Targeted, intensive yet safe exercise requires joint isolation
There is an ongoing discussion about the best kind of exercise in rehabilitation, should it be functional or isolated. There is a place for both but if you have a painful joint with poor coordination and lack of strength there is no other way to provide adequate level of intensity in the exercise in a safe way than using isolated movements.

We can again use the rubber band as an example in the external rotation of the shoulder. How do you make sure that exercise is effectively targeting infraspinatus and teres minor muscles? You cannot. Especially when pain is involved, patients will use any muscles they can trying to minimise the movement that produces pain.
With a proper fixation, correct resistance curve and visual guidance patients will automatically exercise correctly and use the right target muscles. This allows early activation of even painful joints with high level of precision. This also quickly empowers the patient as they learn that movements are not painful. This will boost their motivation to exercise, which is a critical success factor.
4. Data-driven individualization enables dosage-based exercises
Our slogan is “movement as medicine”. Medicine is prescribed accurately for each patient and only pill taken has the desired effect. But most exercises are not dosage based. It is practically impossible to fully control the parameters of typical exercise programs. Here is a list (not complete) of parameters that need to be controlled:
- Type of exercise (device / tool used)
- Resistance level (as percentage of 1RM= Repetition Maximum)
- Distribution of resistance over the range of movement
- Range of motion (start angle, end angle)
- Speed (degrees / second)
- Repetitions (workload)
- Change in resistance (progression)
- Change in range of motion
- Number of sets / each exercise
- Session / week
- Number of sessions
- Additional exercises, relaxation, psychological intervention
One can only imagine how many different variations are possible. Who is to say what is the best combination of exercises, what load levels to use, how much to push without causing more harm than benefit? When you add here the diversity in the patient population, including variation in age, sex, bodyweight, socioeconomic position, psychological profile, pain level, diagnosis, training history and so on, things become incredibly complex. Prescribing exercise without a structured system is a bit like taking a handful of pills randomly.

Program planning starts by analyzing the baseline status of the patient. This includes strength and mobility tests, pain profile and a set of questionnaires and any physical evaluation needed. All information is automatically collected by the software from the devices, tablets, mobile phones or the Info-Kiosk which is part of the set-up.
Based on the collected data the software will automatically plan the individualized program. It will suggest the resistance, speed, repetitions, sets, visit numbers and so on. Therapists can manually change anything, but there is seldom need to do that.

Planning the program is only half of the challenge. The other half is to make sure the pill is taken as prescribed. One part of that is to guide the patient to perform everything correctly and the other part is to control that everything was done correctly. This is achieved with a very motivating interactive display. Patient knows exactly what to do, how to do and then get immediate feedback how well it was done. The screen shows the patient how well the movement was within limits and what the so-called “compliance” was. The power of this visual guidance is quite amazing. The average compliance of all exercises in all clinics is 92%.
This means that not only is the system’s ability to prescribe individual dosages accurately unprecedented but also its ability to motivate and control the patient is unique.
5. Exercises are measurable
Monitoring all exercises digitally real-time and collecting the data serves many purposes. On the patient level it is a requirement to provide visual guidance and quality feedback. For the therapists it an invaluable tool to ensure treatment quality and to target help and advice to those that really need it. Collected exercise data together with the patient’s feedback on the resistance and pain levels are used to automatically change the exercise parameters for the next session.
Patient or group level reporting is easy with all the data available. In addition to outcome reporting also individual sessions can be reported with a click of a button down to the smallest detail. Insurance companies can see exactly what the patient has done, not only generic descriptions.
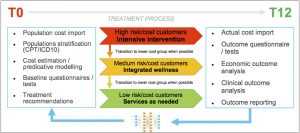
On a larger scale data serves as the basis of all development, provides material for scientific studies and is the food for the insatiable AI -engine. The picture below describes how the data is used in the development of population health programs.
6. Intelligent devices can empower patients to independence
One factor in healthcare is always an issue: money. There is simply not enough money to treat everyone optimally. And the future looks even bleaker. Populations get older, people move less, and costs are soaring. When it comes to musculoskeletal problems, it is simply not possible that there is a therapist for every patient for as many session as needed.
There has to be another way. And there is. We have seen that it is very easy to empower patients to become self-reliant after two-three individual sessions. When the program is settled after the initial fine-tuning, patients can manage with very little supervision. The system allows one therapist to treat up to 6 patients at the same time providing substantial cost savings. Read here how the role of therapists in St. Lucas was changed, productivity increased while medical outcomes improved when they adopted our intelligent system.
And there is an added bonus here: every government in the world would be drooling over a method that can pull patients out of the healthcare system and convert into self-caring individuals. This is what our solution has demonstrated. People become more interested in their own health and now they know how to take care of it. Self-training has become and important additional income source for many centers. Patients are converted to members who pay monthly fees and visit the center once or twice a week to maintain their health.
7. Cloud-based system broadens control and applications
There are many compelling reasons why the system should be controlled in the cloud. Cloud-based system allows easy access for the management to all relevant data regardless of the location or how many clinics are under management. Management is transparent, effective and real-time.
With the cloud-based system patients can visit any location in the chain. One scenario is where a rehabilitation unit is in a hospital and a stand-alone prevention unit in another place closer to patient’s home. Programs are always available and updated regardless of the location visited.

Treatment program should include more than just the visits at the clinic. For a 360-degree view of the patient data must be collected independent of location. This involves monitoring home exercises, general activity and even sleep. Also, communication with the patient via an app is part of the process. Integration of this data outside the clinic requires cloud-based functionality.
For mission-critical technology like this up-time and data integrity are critical. With the cloud-based solution clinics can forget about server issues, back-ups and software updates. Past nine years have proven that a cloud-based solution can be very reliable and trouble free solution.
Conclusion
Exercise therapy is, without a doubt, going to become one of the key disciplines in healthcare. Everyone operating in this space should be able to provide answers concerning these 7 points. Skilled therapists can offer safe and beneficial exercises even with limited tools. But for the quality and patient safety it is important to make a clear distinction between medically qualified device-based exercise and fitness training. Although there may be superficial similarities we are talking about two totally different things. Proper device-based exercise therapy is carried out with medically certified technology with validated protocols and supervised by licensed physical therapists specially trained for this.
The fact that device-based exercise therapy is going to gain ground in the medical world is already clear. National level insurance reimbursements and contracts with health ministries in different countries are a proof of that. When people become more familiar with these ideas and have a chance to personally try in practice how the system works, attitudes will change. Therapists, who may feel threatened by these new ideas quickly learn to embrace them after seeing how it changes their work for the better. For doctors we have seen that an effective way to convince them is to ask them to “send their worst” and see the client outcomes and reactions.
 English
English 
























