Preliminary Data Overview
Participants: 447 individuals (mean age 49.9 years) with chronic back or neck pain
Setting: Three rehabilitation facilities in the Netherlands
Intervention: 12-week individualised DAVID Spine program (2–3 sessions per week)
Assessments: Pain (VAS), function (ODI/NDI), kinesiophobia (TSK), isometric trunk strength, and lumbar range of motion (ROM)
Key Findings
1. Functional improvement was remarkable
-
ODI (Low back pain): average decrease of −5.9 points (large effect size d = 0.91)
-
58% of patients showed ≥30% functional improvement
-
-
NDI (Neck pain): average decrease of −3.1 points (moderate effect size d = 0.60)
-
35% achieved ≥30% functional improvement
-
2. Fear of movement significantly decreased
-
The Tampa Scale of Kinesiophobia (TSK) dropped by around 5.5 points on average (d = 0.8–0.9).
-
Reduced movement fear likely contributed to better adherence and continued progress.
3. Strength gains were substantial
-
Isometric trunk strength improved significantly in all six Lumbar movement directions, with a median effect size of 1.13 (large).
-
The most notable gains were seen in rotation and lateral flexion—key stabilising movements for daily function.
4. Pain levels improved modestly
-
Average back pain reduction was −0.7 points on a 10-point VAS scale, though about one-third of participants experienced a clinically meaningful (≥2-point) improvement.
-
For neck pain, the group average remained stable, but nearly one-third still reached meaningful relief.
5. Range of motion changes were direction-specific
-
Rotation and lateral flexion to the right increased notably (+9.2° and +6.5°), while small decreases were seen in left rotation and extension.
-
These findings may inform future optimisation of progression patterns in training protocols.
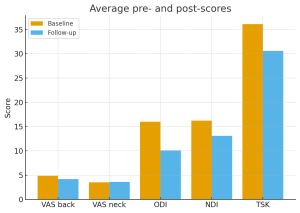
Figure 1 – Average pre- and post-scores (VAS back/neck, ODI, NDI, TSK)
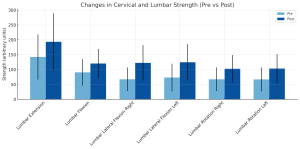
Figure 2. Changes in Lumbar Strength (Pre vs Post).
Mean (±SD) values for lumbar extension, flexion, and rotation right strength are shown before (Pre) and after (Post) participation in the DAVID Spine training program. All strength directions demonstrated statistically significant improvements (p < 0.001, paired t-tests).
Real-World Evidence Matters
This analysis stands out because it reflects routine care data, not controlled lab conditions. The findings show that even in everyday clinical practice, a standardised, data-driven DAVID Spine program can produce meaningful functional recovery for people with chronic back and neck pain. While pain relief alone may vary between individuals, improvements in disability, fear of movement, and trunk function reflect the core goal of modern rehabilitation: restoring capability and confidence.
Looking Ahead
The authors conclude that approximately one-third to one-half of patients reached clinically meaningful thresholds across outcomes, a strong indication of program effectiveness. Further prospective and controlled studies are underway to validate these findings and deepen understanding of how device-guided rehabilitation can best serve diverse patient populations.
About the DAVID Spine Concept
The DAVID Spine Concept combines biomechanically precise devices, intelligent software, and evidence-based protocols to restore spinal function safely and effectively. With real-time feedback, measurable outcomes, and progressive loading, the system empowers both therapists and patients to track recovery objectively and achieve sustainable results.
References
Babatunde, O. O., Jordan, J. L., Van der Windt, D. A., Hill, J. C., Foster, N. E., & Protheroe, J. (2017). Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLOS ONE, 12(6), e0178621. https://doi.org/10.1371/journal.pone.0178621
Kankaanpää, M., Taimela, S., Airaksinen, O., & Hänninen, O. (1998). Back and hip extensor fatigability in chronic low back pain patients and controls. Archives of Physical Medicine and Rehabilitation, 79(4), 412–417.
Kankaanpää, M., Taimela, S., Airaksinen, O., & Hänninen, O. (1999). The efficacy of active rehabilitation in chronic low back pain: Effect on pain intensity, self-experienced disability and lumbar fatigability. Spine, 24(10), 1034–1042.
Kujala, U. M., Taimela, S., Videman, T., Battie, M. C., & Viljanen, T. (1996). Physical loading and performance as predictors of back pain in healthy adults: A 5-year prospective study. European Journal of Applied Physiology, 73(5), 452–458.
Leinonen, V., Kankaanpää, M., Luukkonen, M., Hänninen, O., Airaksinen, O., & Taimela, S. (2003). Lumbar paraspinal muscle function, perception of lumbar position, and postural control in disc herniation-related back pain. Spine, 28(8), 842–848.
Leinonen, V., Määttä, S., Taimela, S., Herno, A., Kankaanpää, M., Partanen, J., Kansanen, M., Hänninen, O., & Airaksinen, O. (2002). Impaired lumbar movement perception in association with postural stability and motor- and somatosensory-evoked potentials in lumbar spine stenosis. Spine, 27(9), 975–983.
Mannion, A. F., Müntener, M., Taimela, S., & Dvorak, J. (2001). Comparison of three active therapies for chronic low back pain: Results of a randomized clinical trial with one-year follow-up. Rheumatology, 40(7), 772–778.
Mannion, A. F., Taimela, S., Müntener, M., & Dvorak, J. (2001). Active therapy for chronic low back pain: Effect on back muscle activation, fatigability, and strength. Spine, 26(8), 897–908.
Mannion, A. F., Junge, A., Taimela, S., Müntener, M., Lorenzo, K., & Dvorak, J. (2001). Active therapy for chronic low back pain: Factors influencing self-rated disability and its change following therapy. Spine, 26(8), 920–929.
Müller, G., Pfinder, M., Clement, M., Kaiserauer, A., Deis, G., Waber, T., Rieger, S., Schwarz, D., Heinzel-Gutenbrunner, M., Straif, M., Bös, K., & Kohlmann, T. (2018). Therapeutic and economic effects of multimodal back exercise: A controlled multicentre study. Journal of Rehabilitation Medicine, 50(10), 902–910. https://doi.org/10.2340/16501977-2497
Peolsson, A., Öberg, B., & Hedlund, R. (2001). Intra- and inter-tester reliability and reference values for isometric neck strength. Physiotherapy Research International, 6(1), 15–26.
Rissanen, A., Heliövaara, M., Alaranta, H., Taimela, S., Mälkiä, E., Knekt, P., Reunanen, A., & Aromaa, A. (2002). Does good trunk extensor performance protect against back-related work disability? Journal of Rehabilitation Medicine, 34(2), 62–66.
Taimela, S., Didrich, C., & Heinrichy, M. (2000). The role of physical exercise inactivity on low back pain recurrence and absenteeism from work after active outpatient rehabilitation for recurrent-chronic LBP: A follow-up study. Spine, 25(14), 1809–1816.
Taimela, S., Takala, E. P., Asklöf, T., Seppälä, K., & Parviainen, S. (2000). Active treatment of chronic neck trouble: A prospective randomized intervention with multi-modal treatment emphasizing proprioceptive training and activated home exercises. Spine, 25(8), 1021–1027.
Taimela, S., Härkäpää, K. (1996). Strength, mobility, their changes and pain reduction in active functional restoration for chronic low back disorders. Journal of Spinal Disorders, 9(4), 306–312.
Taimela, S., Negrini, S., & Paroli, C. (2004). Functional rehabilitation of low back disorders. European Journal of Physical and Rehabilitation Medicine, 40, 29–36.
Taimela, S., Kankaanpää, M., & Luoto, S. (1999). The effect of lumbar fatigue on the ability to sense a change in lumbar position: A controlled study. Spine, 24(13), 1322–1327.
Ville Leinonen, M. D., Markku Kankaanpää, D. M. Sc., Matti Luukkonen, M. D., Martti Kansanen, D. M. Sc., Osmo Hänninen, D. M. Sc., PhD, Olavi Airaksinen, D. M. Sc., & Simo Taimela, D. M. Sc. (2003). Lumbar paraspinal muscle function, perception of lumbar position, and postural control in disc herniation-related back pain. Spine, 28(8), 842–848.
 English
English 
























